A mother is very happy when she comes to know that she is going to give birth to twins, but on the other side, twin pregnancies come with more risks and challenges for mothers, babies, and doctors. Twin-to-twin transfusion syndrome occurs when both the twins share a common placenta.
What is Twin-to-Twin Transfusion Syndrome (TTTS)?
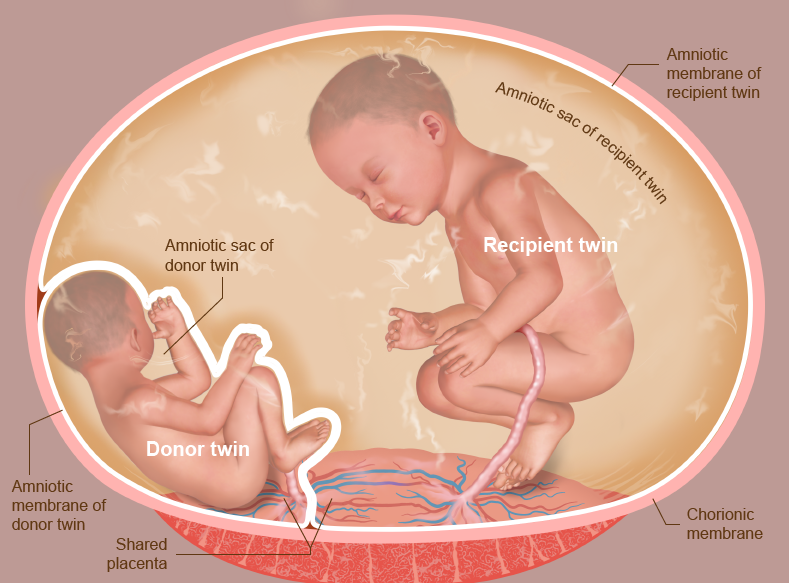
It is a disorder in which identical twin pregnancies are affected. This syndrome occurs when a single placenta is shared by two fetuses (referred to as a monochorionic twin pregnancy) because no barrier can separate the two fetuses from each other.
Sometimes, abnormal connections are formed within the shared space of twins by the blood vessels from the twin’s umbilical cords that connect one baby to the other. Due to this, there is uneven blood flow between the babies and their circulations become unbalanced. This leads to the early delivery of twins, neurological damage, and more.
Twin-to-twin syndrome is a serious condition and rare, which is only seen in identical twins who share a placenta (monochorionic). One fetus is the donor who donates blood and fluid to the other fetus known as recipient. Due to this, the production of urine stops in the donor fetus and its amniotic sac becomes much smaller.
In the recipient twin, the amniotic sac will be large because it receives too much blood and urine and produces more amniotic fluid. There can be severe complications in twins due to TTS. That’s why early detection of TTS can be helpful for both the babies and their mothers.
What Causes TTTS in Pregnancy?
The exact cause of TTTS is not known, there are no genetic and maternal causes of TTTS. TTTS develops in the second trimester of pregnancy in the majority of cases.
There is nothing anyone can do to prevent TTTS, but there are many things we can do to help our babies. When twins are monochorionic-diamniotic it is important for families that early surveillance for TTTS should be done specifically by having ultrasounds every two weeks starting at 16 weeks of gestation.
Who Gets TTTS?
Identical twins are affected by TTTS before they are born. Out of 250 pregnancies, every one pregnancy is identical or monochorionic and approx two out of three pregnancies are monochorionic diamniotic, which means the fetuses share a common placenta but have two separate amniotic sacs. About 10 to 15% of these pregnancies develop TTTS.
TTTS can happen in monochorionic monoamniotic twins, in which the twins are in one sac without a dividing membrane.
Symptoms of TTTS
Mothers may not experience symptoms of TTTS in many cases. But some mothers whose twins have TTTS will feel signs of excess amniotic fluid.
Signs and symptoms a mother may experience are as follows:
- Larger uterus for her stage of pregnancy
- She feels that her abdomen is growing or expanding rapidly
- A sudden increase in her body weight
- Increased abdominal pressure
- Abdominal pain
- Difficulty in breathing
- Cramps and contractions in the uterus
- In early pregnancy, there is swelling of hands and legs
If a woman is pregnant and experiences any of the above symptoms, then she should consult her doctor immediately for further evaluation.
Stages of Twin-to-Twin Transfusion Syndrome
Quintero staging system is used to stage TTTS in which there are five stages and among them, the most serious stage is the fifth one.
Following are the stages of TTTS:
Stage 1: In this stage, there is a significant difference in amniotic fluid volume in each twin’s sac.
Stage 2: In this stage, the bladder of the smaller baby is not visible by ultrasound.
Stage 3: There is abnormal blood flow through the umbilical cord and fetal vessels around the heart.
Stage 4: A condition known as hydrops develops in which there is an abnormal accumulation of fluid in more than one body cavity. This can be seen in one or both twins.
Stage 5: In this, there can be the death of one or both twins.
By using the Cincinnati staging system we can further categorize the severity of the baby’s heart condition as mild, moderate, or severe and this will depend on results of the fetal echocardiography.
The patient meets with members of the team after the test results are available, which includes a maternal-fetal medicine specialist, a surgeon, and a nurse.
Diagnosis of Twin-to-Twin Transfusion Syndrome
Twin-to-twin transfusion syndrome can be suspected by a doctor based on the results of routine prenatal ultrasound. Detailed testing to measure amniotic fluid volume, bladder filling and blood flow in the recipient and donor twins can be conducted by a maternal-fetal medicine specialist to confirm the diagnosis.
The mother is at risk of preterm labour and there can be a shortening of the cervix when there is a rapid increase of amniotic fluid volume because by this the uterine cavity also expands at an accelerated pace. This situation may lead to preterm labour or preterm rupture of membranes after delivery. Because of this in all women presenting with suspected TTTS maternal assessment of cervical length and the uterine cavity is essential.
Cardiovascular dysfunction in the twins is an important factor in determining the prognosis of TTTS. That’s why a detailed examination of the fetal heart (fetal echocardiography) in both recipient and donor should be done to diagnose TTTS.
Treatment of Twin-to-Twin Transfusion Syndrome
Early diagnosis and intervention is the key to treat twin-to-twin transfusion syndrome. Treatment options vary according to the stage of the TTTS and the gestational age of the baby. Following are the treatment options:
- Expectant management: Expectant management is recommended for stage 1 TTTS. Ultrasound and fetal echocardiography should be done throughout the pregnancy to monitor the babies. Surgery is not needed in less severe cases.
- Amnioreduction: In this, the excess amount of amniotic fluid that is accumulated in the amniotic sac of the recipient twin is removed. The doctor uses “real-time” ultrasound images to guide a long, very fine needle into the uterus to withdraw the fluid. This is similar to amniocentesis. This is recommended in stage 1 of TTTS and when the TTTS is diagnosed late in the pregnancy.
- Fetoscopic laser photocoagulation: It is the minimally invasive surgery in which a laser is used to ablate the blood vessels that are contributing to the abnormal blood flow to the babies. According to some studies, this is the most effective therapy for babies with advanced TTTS.
- Delivery: Delivery may be the best option when TTTS is discovered late in the pregnancy.
Sources: